The Gaps in Hard Tissue Surgical Robotics
Surgical robotics has revolutionized soft tissue procedures, improving precision, reducing recovery times, and enhancing outcomes. Yet, in hard tissue robotics, progress has lagged behind. Orthopedic and spine surgeries require the same level of innovation, yet existing robotic solutions fail to meet the full spectrum of clinical needs.
Hospitals are investing in multiple robotic platforms—one for knee replacements, another for spine, yet another for shoulder—leading to inefficiencies in cost, training, and workflow. Surgeons are forced to work with rigid, single-application robots that often limit flexibility and increase operational complexity.
The demand for more versatile, intelligent, and cost-effective robotic systems in hard tissue surgery is growing, and the industry must catch up. Let’s explore the unmet needs preventing surgical robotics from reaching its full potential in orthopedic and spine surgery.
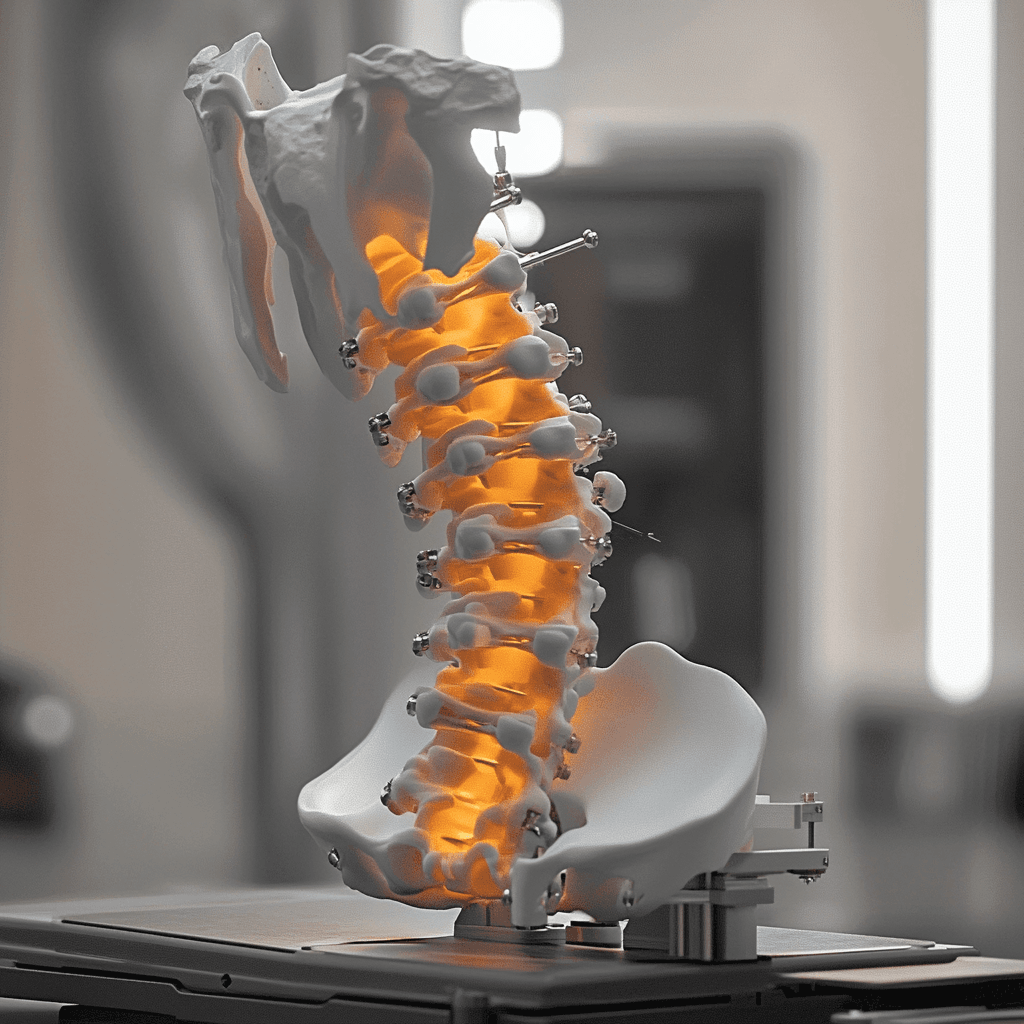
Why Has Hard Tissue Surgical Robotics Fallen Behind?
Limited Versatility and Single-Purpose Systems
- The Problem: Hospitals must purchase multiple robotic systems for different types of surgeries, increasing capital investment while reducing return on investment (ROI).
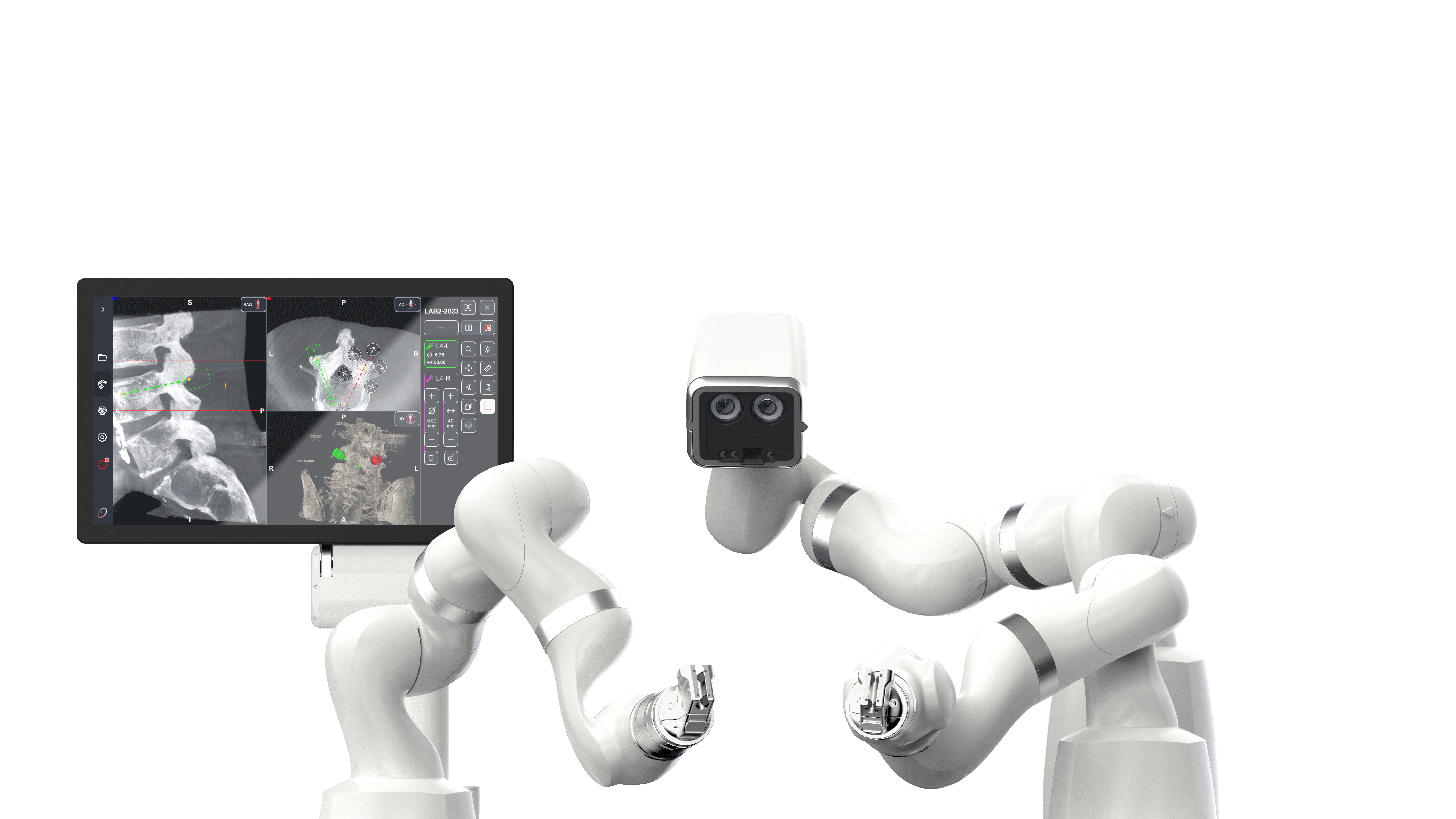
- The Opportunity: Agnostic, multi-functional robotic platforms that can handle various orthopedic and spine procedures would reduce the need for multiple devices and increase surgical flexibility.
Locked Ecosystems and Implant Restrictions
- The Problem: Major players like Stryker, Zimmer, Medtronic, and Globus require hospitals to use only their implants with their robotic systems. This restricts surgeon choice and forces hospitals into expensive, long-term contracts.
- The Opportunity: A robotic system that works with multiple implant brands would give hospitals and surgeons greater freedom, lower costs, and more control over their surgical workflows.
Poor AI Integration and Learning Capabilities
- The Problem: Many existing robots rely on static preoperative planning, without the ability to adapt in real-time based on anatomy changes during surgery.
- The Opportunity: AI-driven robotics with machine learning capabilities could allow for more adaptive decision-making, reducing human error and increasing procedural efficiency.
Lack of Workflow Efficiency and Surgeon-Friendly Design
- The Problem:
- Long setup times slow down operating room (OR) efficiency.
- Steep learning curves increase the need for extensive training.
- Lack of interoperability with existing hospital systems leads to data silos.
- The Opportunity:
- Ergonomic, easy-to-use robotic systems with intuitive interfaces.
- Seamless electronic health record (EHR) and imaging system integration for real-time surgical planning.
- Faster onboarding and training, reducing downtime and improving OR productivity.
High Costs and ROI Concerns for Hospitals
Robotic-assisted surgery in hard tissue applications is often seen as a high-cost, low-return investment because current solutions lack broad applicability.
- The Problem: Many hospitals cannot justify the cost of a robotic system that only performs one type of surgery.
- The Opportunity: A modular, cost-effective robotic platform that can be scaled for multiple applications could dramatically improve ROI and increase adoption across hospitals of all sizes.
How the Industry Must Evolve
The next generation of hard tissue robotics must prioritize the following:
- Multi-Application Use: A single robotic platform that can handle multiple orthopedic and spine procedures, reducing hospital costs and improving efficiency.
- Implant-Agnostic Design: A system that works with multiple implant brands, giving surgeons greater choice and control over surgical outcomes.
- AI-Powered Real-Time Adaptation: Robotics that respond dynamically to intraoperative changes rather than relying solely on preoperative planning.
- Surgeon-Centric Usability: More intuitive controls, faster learning curves, and better OR integration to reduce disruption and improve workflow.
- Scalable Cost Models: Flexible purchasing and subscription-based models to lower barriers to adoption.
The industry is on the verge of a major shift. Hospitals, surgeons, and technology innovators must work together to create robotic solutions that meet the evolving demands of orthopedic and spine surgery.
The Future of Hard Tissue Robotics
Join the Conversation
- Want to stay ahead in surgical robotics?
- Join the conversation and explore the future of robotics with us.
